January 13, 2025
MWHS Leadership Spotlight
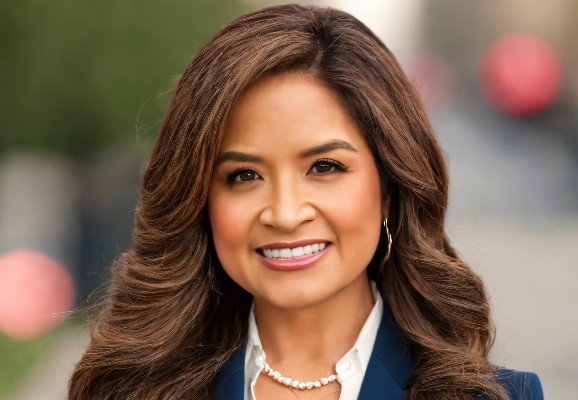
April Joy Damian, PhD, MSc, CHPM, PMP, is a distinguished psychiatric epidemiologist and a leader in health services research. She serves as Vice President and Director of the Weitzman Institute, the research, education, and policy arm of the Moses/Weitzman Health System. In addition to her leadership role at the Weitzman Institute, Dr. Damian is the Health Equity Senior Scholar in Residence at AcademyHealth and holds a faculty appointment at the Johns Hopkins Bloomberg School of Public Health. In this interview, she reflects on her roots and shares insights into her work related to youth mental health. Dr. Damian describes some of the innovative programs at the Weitzman Institute and discusses why primary care is the cornerstone of the U.S. healthcare system. This interview has been shortened and edited for clarity.
Dr. Damian, what first drew you into the health field?
I grew up in San Francisco. Both of my parents migrated from the Philippines. I understood early that health is wealth, and that health affects everything we do in life—how we show up to work, to school, and in our relationships, personal and professional. It’s not just about healthcare, but health and wellbeing. As a child, I saw in my own family and community that certain populations were more impacted than others in terms of access to opportunity and having a great quality of life.
I often talk about my dad. He had multiple chronic health conditions. As a child, I saw him in the ICU. I could tell that he was in pain but couldn’t really express it. I think it caused him mental distress to express his emotions and his suffering. This was a mental health issue. My direct observations over time shaped my understanding of health. This is what we mean by “lived experience” and “embodied expertise.” My formal academic training introduced me to research to back up what I already knew from direct observation. Also, my parents taught me that if you see something, say something. If there is an issue or a challenge, it’s your job to be part of the solution.
You are a “psychiatric epidemiologist.” Tell us how those two fields come together in your work.
Epidemiology offers a public health orientation. We look at disease of whole populations. As a psychiatric epidemiologist, I am interested in the mental health of whole populations. For example, if you think of anxiety, depression, alcohol, substance use disorders—what is their prevalence, and what does the trajectory look like in different populations? My scholarship has largely focused early in the life course, particularly adverse childhood experiences (ACEs), childhood trauma, and the response of systems to mental health disorders related to ACEs. Clinicians largely focus more on the individual in front of them. My training complements this work by examining how we can look at mental health from a population standpoint.
How does this include the social drivers of health, the societal issues that affect people’s mental health?
Beyond what a clinician might see within the four walls of their clinic, there is a larger context in which individuals, families and communities live, breathe, play, pray, work and age. These are what we call the “social drivers” of health, or the “upstream” factors.
For example, how do issues such as racism, climate change, access to employment, and food insecurity affect people’s mental health? Some people are living in food deserts, others in areas of food abundance. How does the experience of being excluded affect one’s mental wellbeing? We talk about climate change and climate anxiety. What happens to our mental health when we live in areas near toxic dumps? How does urban design, such as freeways, breaks up communities and affect social cohesion? I’m always thinking about how all of these factors interplay when it comes to the mental health of whole populations. What does it look like when you don’t have access to green spaces? When you can’t put food on the table for your kids? All of these things impact our mental health.
How do you decide what to prioritize in your work?
It’s a great question. There is no shortage of issues that keep me up at night. We have to start somewhere. First, I lean on my strengths. I have largely focused on youth and adolescents. How do I lean into my strengths and go deeper in those areas, while also turning to my colleagues who are knowledgeable about other areas? At Weitzman, we largely focus on the context of safety net primary care. That’s the area where I live and breathe right now. I think it’s important to ask what we can do ourselves, and where to lean into the strengths, expertise, and passion of our colleagues. When we do that, we can address the issues in a more comprehensive way.
“Beyond what a clinician might see within the four walls of their clinic, there is a larger context in which individuals, families and communities live, breathe, play, pray, work and age.”
Dr. April Joy Damian
The U.S. Department of Justice recently awarded the Weitzman Institute a grant to evaluate a special youth program. Tell us about this project.
I’m really excited to serve as the Principal Investigator for this DOJ-funded initiative. Heal Our Youth is a ten-week, restorative justice and mindfulness program. It was initially designed by Active Plus, a New York-based nonprofit. They work in all five boroughs. We know there’s a huge need in terms of addressing childhood trauma among our health center populations. Not all of the issues can, or should, be addressed in a clinical setting. We also know that the demand for trauma-informed mental health services exceeds the supply. The question becomes, how are we supporting young people beyond their clinical visits?
I appreciate several things about Heal Our Youth. One, it takes a strengths-based approach. So much of the way we address mental health in the U.S. is a deficit approach—what’s wrong with the person? Heal Our Youth turns that around by asking, how are we building resiliency and community? How are we leaning into community assets, in addition to the assets of the individual youth, to be able to promote their thriving?
Second, we’re still recovering from the COVID pandemic. We’re not in the surge, but in terms of the psychosocial impact, we are still in it. Youth development and learning have been disrupted. How are we promoting their connection with themselves, but also with each other? This program really allows them to engage in-person with other youth and with trusted adults.
Third, we are in a youth mental health crisis. The younger generations are leading the way in terms of normalizing conversations about mental health, addressing it openly, and being vulnerable when it comes to their mental health. How are we, as adults, embedding programs in the community to support what young people are already calling for?
Heal Our Youth teaches restorative justice and mindfulness techniques. In Connecticut, we are implementing the program at one of our sites. One of the participants told us, ‘I was getting so angry at a classmate, then I decided to sit outside of the classroom, take a deep breath and just collect myself.’ And it worked. Once young people learn these techniques, they can use them anywhere, and it doesn’t cost anything. The student is now able to bring that skill with them into adulthood, even share with peers and family members. The multisite randomized controlled trial, the gold standard for evaluating the effectiveness of interventions, will give us the opportunity to look at the program in depth, to better understand how it works. We are grateful to the Department of Justice for its support.
What else is happening at Weitzman this year?
So much! We have over three dozen research, education, and policy projects going on across our key focus areas of social determinants of health, workforce development, and systems transformation. In 2025, we are emphasizing mental health. It’s the line that connects the dots across our portfolio. We have a wonderful program called Prescription for Play (P4P), funded by The LEGO® Foundation. P4P uses play as a tool to promote healthy parenting in the pediatric well-child visit. We have distributed over 2.5 million LEGO play kits and worked with close to 5,000 medical professionals across all 50 states, Puerto Rico, and the U.S. Virgin Islands. P4P fits with our strengths-based approach. It’s not just for kids, but also their parents and caregivers.
We are also taking a close look at chronic disease and prenatal and maternal health. Maternal health intersects with mental health. In our ECHO virtual education program, we will be supporting rural healthcare providers who work with mothers.
Recently, we received our first grant from the National Institutes of Health. It allows us to build capacity in the area of alcohol use among medical and behavioral health providers in primary care. We want to make sure our primary care workforce is equipped with the latest, evidence-based treatments and research. We know that alcohol use disorder continues to be a major healthcare and public health issue, and we’re trying to bridge the gap that sometimes exists between health centers and research. It’s a great project, also very much within the mental health space.
Why is primary care so important in terms of the overall health ecosystem?
All of the evidence points to the fact that primary care improves quality of life and health outcomes. It reduces disparities, especially for people who have experienced the greatest inequities. There’s really no conflicting evidence at all. Thinking from a cost containment perspective: Close to twenty percent of the U.S. GDP goes towards healthcare. If quality primary care were accessible to everyone and people went to their primary care visits, one estimate is that we would save 67 billion dollars per year. Just think about that. Even if you aren’t sold by the moral imperative of people living healthy lives and having equitable access, you could be sold on the economics of it. Primary care is the central place where all of this gets coordinated and is the backbone of U.S. healthcare system. We are working in that foundational area of healthcare. I think the potential for large-scale impact is what makes our programs even more important.
As we move into the new year, what inspiration can you share?
I operate in plurality. I know how important it is that we work together. I am committed to recruiting and retaining innovative and committed people who are invested in our mission. I’m fortunate to work with such outstanding colleagues and collaborators. They enable me to lean into my strengths, and I get to work with them and learn from them about the areas where they are strongest. We have a great team, and we share a commitment to contribute in a positive way to the health and wellbeing of others. This is why I’m really excited for 2025 and beyond. We can accomplish so much when we appreciate the strengths of others.
